Raising a Twinless Twin – How TTTS forever changed our Lives
Kathryn’s Story

Our twinless twin
This blog is dedicated to my infant daughter Kathryn, who died two days after birth due to complications from TTTS. She was a special baby, who my husband and I firmly believe stuck around long enough to ensure her identical twin sister could survive. Through this blog I hope to bring more awareness to Twin To Twin Transfusion Syndrome, find an outlet for my grief, and potentially help others along the way! We struggle daily with our loss and raising a “twinless twin” and I hope to find comfort and give comfort in this journey.
Thank you Kathryn, for waking me up!
My husband and I are both the 3rd of 4 children (he of 4 boys, me of 4 girls) so having a 3rd child wasn’t even something we debated – we just knew we had to. When I learned that our 3rd child was actually our 3rd and 4th child, to say I was shocked would be a GINORMOUS understatement! It took months for me to adjust to the idea, and about the time I was getting excited about the idea of identical twin daughters, our nightmare began.
If you know someone who has lost a baby and you are looking for ways to support them, please read this post: The Magic Words When Someone Loses a Baby
I had never heard of Twin To Twin Transfusion Syndrome (TTTS) until I was pregnant with twins, and even then I knew very little. One of the OBs at my clinic vaguely mentioned something in the first appointment. She very nonchalantly mentioned that twin pregnancies in which the babies share aplacenta is higher risk because one twin can sometimes try to take more than their share, but “there are things that can be done” to set everything right again. The OB did not seem all that concerned about it, so neither was I.
TTTS was not mentioned again until that life altering moment in our 20 week anatomy ultrasound when the technician stated: “Do you see this black pocket around Baby A’s belly? That is fluid. The doctor will talk to you more about this in a moment, but your babies have Twin to Twin Transfusion Syndrome.”
And at that moment my life changed…
Our daughters are monochorionic-diamniotic (Mo/Di) twins – one placenta, two sacs. Twin to Twin Transfusion Syndrome (TTTS) occurs in roughly 15-20% of Mo/Di twins, and sadly is the cause of more deaths of babies each year than SIDS, yet have you ever heard of it? We were officially diagnosed with TTTS at 20W and 2 days during our regularly scheduled Anatomy ultrasound (U/S). My doctors notes from that day state: Anatomy u/s today reveals TTTS. One fetus with poly/90% pericardial effusion/ascites. Other baby with oligo/10%. Discordance 46%. Will need to transfer to MFM.” Translated that means – one baby has way too much fluid at 90% and the other has 10% and there is a 46% difference in their sizes. Baby A (Kathryn) was 50% too large at the time and Baby B was 50% too small. Their weight differences were 100% (16 oz and 8 oz.)
The problem with TTTS is that the babies do not receive an even share of the placenta and the fluids for survival. One baby is a donor baby, the other a recipient. The recipient receives excess fluids and this overload can cause heart failure and hydrops, which is what Kathryn developed. Many donor twins also are unable to thrive and die from not receiving enough fluids.
Sadly, as I begged my OB to tell me what we could do, she doctor told me “nothing could be done” to save them. And then she admitted me into the hospital. That day as they wheeled me to Labor and Delivery, I thought I was losing both of my babies. I am sure half of the hospital heard me wailing and sobbing as the Medical Tech wheeled me across the hospital.
Thankfully, that doctor was wrong. And since then I have come to realize that many OB/GYNs know very little about TTTS and because of this lack of knowledge, babies are lost. I will never know if our situation could have been different, but I know that we can work to save other babies.
I digress.
So on September 28, 2011 I was hospitalized immediately. The next morning the Maternal Fetal Manager (MFM or high risk OB/GYN) visited me and began to tell me about our options. We could do nothing, and both babies would die. We could proceed with an amnio reduction (reduction of the fluids in the amniotic sac to try and return the babies to a normal balance) or there is an option of laser surgery. However, the doc told that due to the fact that I had an anterior placenta (on the front of my abdomen in front of my belly button), we were ineligible for the laser surgery, so our only option was amnio reduction. (Turns out this was also incorrect information – many women with anterior placentas are able to pursue the laser ablation surgery. Some have success, some do not, so I do not dwell on this bad information.)
So on Thursday September 29, 2011 we had our first amnio reduction at 20w3d. It was amazing to watch. It was somewhat uncomfortable to have the large needle inserted into my abdomen, but it was cool to watch the babies. For almost an hour they withdrew fluids out of Kathryn’s sac. Kathryn tried several times to grab the tip of the needle. It was cute. 500 ML of fluid was removed from Kathryn’s side of the sac.
Over the next several weeks we held our breath as we waited for time to pass. The doctors told us we had to make it to 24 weeks to even be considered viable, and at that point, that needed to be our main goal. I went on bedrest (as much as a woman with a four year old and an 18 month old can be!) and we visited the doctors every week for ultrasounds. Amazingly, the babies stayed stable. Kathryn’s hydrops (fluid building up around two or more bodily cavities) did not go away, but it remained stable. Baby B was growing very slowly but she continued to grow, her bladder continued to be visible, and although she was “shrink wrapped” in the membrane separating the babies, she was not “stuck.” Her fluids stayed right around 2-3 CM, which was an acceptable amount and allowed her to continue to get nourishment, albeit very little.
At 24 weeks we took a turn for the worse. Kathryn’s heart was worsening… the tricuspid valve was no longer functioning, and the fluid continued to build tremendously. Her abdomen, at 24 weeks measured the size of a baby at 32 weeks gestation. Baby B was still too tiny to be viable, and this was a scary day. We were once again admitted to the hospital, and this time, since we were at the 24 week point, I was put on magnesium sulfate (AWFUL!!!!) and given steroid shots to help prepare their lungs. Three days later, on 10/27 (24 w and 3 Days) we had our 2nd amnio reduction as well as a pericentesis… this time they also stuck a needle into Kathryn’s abdomen and withdrew over 200 ML of fluid out of her belly. The highest risk with these procedures is that they can cause pre-term labor. Also, by introducing a needle into Kathryn’s abdomen, there was a risk of destabilizing her. The little baby (Baby B) still had a 0% of survival if we were to go into labor then, (she was only measuring at 22 weeks) so we waited with great anticipation to see if the procedure would cause premature labor. Thankfully the babies tolerated it well, and I was able to go home that evening.
The following week showed no improvement. Kathryn continued to take on fluids and the little baby was growing very slowly. At our appointment on 11/1 the doctors notes stated: “Baby A has 6.6 Fluid, Baby B had 2.0”; the comment was made that “Twin A has worsening hydrops.” It didn’t look good. All of us cried (the nurse, the u/s tech, me) as the doctor began to offer us other options. One option to consider was going to the Children’s Hospital of Philadelphia (CHOP) to have a tubal ligation – a procedure to terminate Kathryn at this point because she had such a small chance of survival and keeping her alive was threatening the chances for Baby B’s survival. Baby B was still so small, and growing so very slowly.
We said no. I was not going to give up on Kathryn, and besides, there were no guarantees baby B would survive either once her sister was terminated.
On 11/8 baby B’s fluid levels dropped to 1.2 CM. Not good. The intertwin discordance was 70.5%; but worse, reverse end diastolic flow (REDF) was identified. In a nutshell, she was starting to return fluids back (reverse flow) and this was very bad. We were once again admitted to hospital – and this time we believed delivery was imminent.
However, the babies had other plans in mind. Over the next 32 days, I remained hospitalized on fluids and oxygen, and tons of protein. As long as the babies continued to stay stable, we were just going to leave well enough alone. We did have weekly amnio reductions, and another pericentesis (aspirations of ascites) to draw fluids from Kathryn to allow her lungs to try to get bigger. The doctors didn’t really like to talk percentages with me when it came to survival. And when they stopped talking about other options of treatment for Kathryn (at one point they were considering a transfer to MUSC so that she could have surgery on her heart after birth) I knew that they had little hope for her.
After we got to about 28 weeks and Baby B was finally over 500 grams, the doc finally started saying he thought Baby B would now have about an 80% chance of survival. He never talked about Kathryn.
On 12/10 (30 W and 5 days) I began having large contractions and went into labor. In the best interest of the babies, I had an elected cesarean following the diagnosis of preeclampsia and nonreassuring fetal heart rate testing.
Baby B was actually born first, and from then on became baby A, or “Tiny” as she is referred to in this blog. She weighed 1lb 10 oz but breathed on her own and actually cried at delivery. Kathryn weighed 4lb 5 oz (largely due to excess fluids) but was not breathing. Because Kathryn’s swollen belly took up so much room, her lungs were way too small for her body, and she had to be resuscitated and intubated. Although they were able to somewhat stabilize her for the next 24 hours, they were unable to stop the fluid from continuing to build up, and her arterial blood pressure remained too low. Despite a good fight, Kathryn died on day 2 of life (after 52 hours) “with complications of respiratory distress and congenital heart disease.” Her death certificate however directly states cause of death as “hydrops fetalis.”
Tiny spent 84 days in the NICU, and other than some eating issues that have since resolved, she has been doing great. My new motivation in life is to bring awareness, educate the medical community, and do what I can to help influence more research toward hydrops.
Awareness is so important. Please consider taking the time to read some of our featured TTTS Stories.
I firmly believe if I had been more educated (about signs, symptoms, anything!) and if my doctors had been more proactive, we could have had a different outcome. I can’t tell you for certain that Kathryn would have lived if we had identified the TTTS earlier on, but you can’t tell me that she wouldn’t have. If I had known to pick up the phone and call Mary at the TTTS foundation… could she have put me in touch with a different specialist that would have taken a different approach and saved the babies?
I’ll never know.
Instead what we know is the life of raising a twinless twin. It’s very difficult to work through the emotions of this situation, and I will do all that I can to try to help others avoid something similar.
I can’t change our story, but I can sure try to change someone else’s!
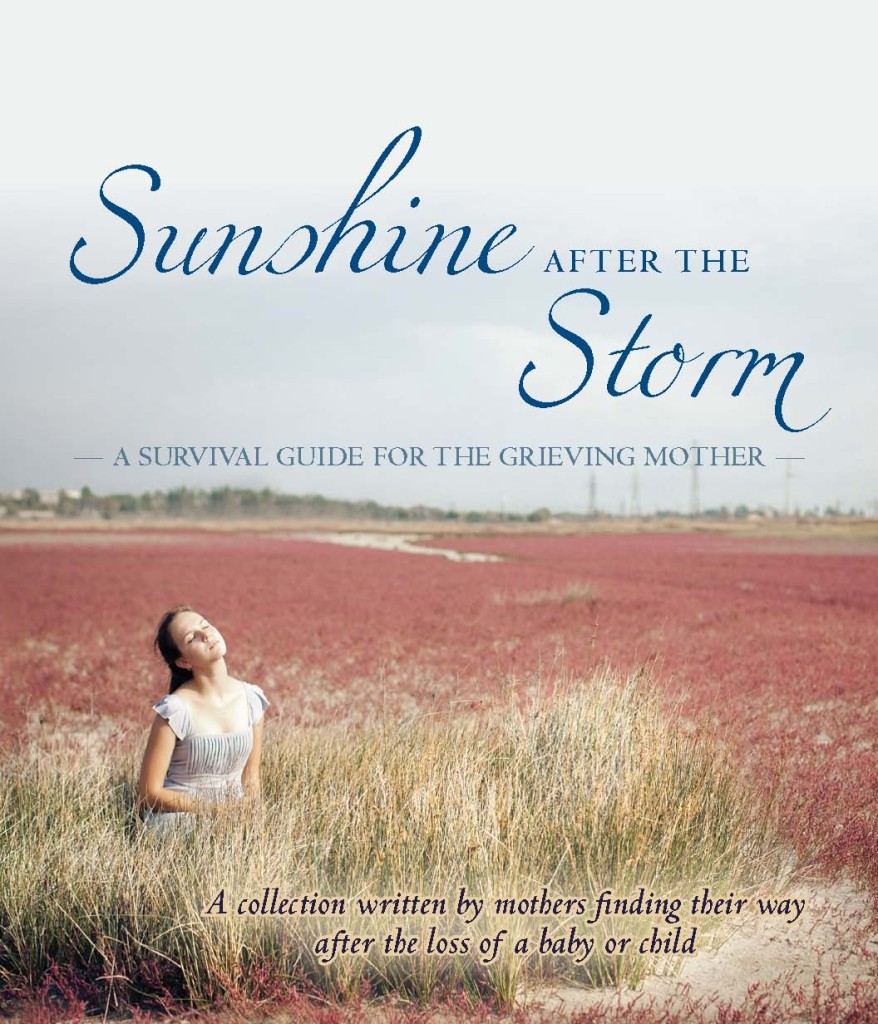
If you know, or someone you know has lost a baby or a child, I encourage you to look into Sunshine After the Storm: A Survival Guide for the Grieving Mother. Written for grieving mothers, by grieving mothers (and some fathers) – this book is a look straight into the soul of over 3o parents who have suffered through this pain and come through it, forever changed.
You can see the book on Amazon here or
Visit the website Sunshine After the Storm, Inc to find out more.